At the start of this week, my leg was a blue and purple haze of bruising.
I was supposed to have the staples removed from my scar 10-12 days after the surgery - so I booked into have them removed by my Wellington based GP on 14 November. However, in the very early hours of that morning, we were awoken by a massive 7.8 earthquake and this was followed by a cascade of significant aftershocks. Being rather slow moving at the moment, I dressed as fast as possible in case we had to evacuate to higher ground because of the tsunami threat. But luckily the threat to our area in Kapiti was downgraded. I am also please that our house was unscathed by the movement. However, the central business district of Wellington was closed for the day while buildings (including the GPs premises) were checked for damage. (If you want to know more about the earthquake - here is a link https://en.m.wikipedia.org/wiki/2016_Kaikoura_earthquake)
Ordinarily, there would be no problem rescheduling the staple removal by a day, however over the weekend, I had developed a red lump under my bra strap and I wanted to get the doctor to check it out as I was concerned it was developing into a red and inflamed boil. So I sent an email and photo off to my GP and asked if she thought it could wait til she saw me. We agreed that it should be ok until the next day. However, Tuesday was a day of torrential rain. So much rain and flooding that all the roads and transport options into Wellington were closed.
I sent an update photo to the GP who said she thought I needed some antibiotics as she was concerned that the boil was getting bigger and she didn't want to risk any chance of infection transferring to my prosthetic. (This is one of the rare but severe risks associated with joint replacement).
I tried to phone a local GP but they didn't answer any of the four calls I made to their clinic. So in the end, I phoned my friendly neighbour Colin (he is a doctor) and asked him for a script for antibiotics. He kindly provided one and then we set off in the pouring rain to get the medicines. Even though we were travelling away from Wellington, what should have been a 20 minute round trip turned into a 2.5 hour trip. Later that evening my GP phoned and said that she had looked at the photo again and thought I should lance the boil with a sterilised needle. Yik. Well - I tried but wasn't very successful at getting the pus out. So decided that I would just have to hope and pray I could get to the doctor the next day.
On Wednesday the roads were still blocked but luckily we were able to get through the road blocks to Wellington to see the GP for our third rescheduled appointment. After a rather brutal encounter with a scalpel, the GP lanced the boil. Overall she was very impressed with the progress with the knee replacement and thought that I was moving well and that the leg wasn't too inflamed or swollen. Then it was off to see the nurse to have the staples removed. I was again surprised at what a long and painful process it is - it took over half an hour. Thankfully this time the scar was well healed and the nurse didn't have to dig into the flesh to pull out bits of metal (like she had to with the right knee).
The scar is dry and isn't as oozy as the right knee scar was. The scar has been covered in steri-strips and a bandage which has to stay on for five days... And then I can have a bath 😄
My sleeping is progressing well. I have tentatively tried sleeping on both sides and I can now creep to the toilet in the middle of the night without clomping around on my crutches.
I am getting more confident walking around the house unaided for very short periods of time and the rest of the time I am just using one crutch. I still use both crutches outside. Yesterday I wandered around for 2.5kms
The knee and leg are still painful so I haven't started to reduce my pain meds yet. But it is tolerable.
We came back home on Thursday and I was not too uncomfortable managing the 2.5 hour trip in the car. It is great to be home and to be out of the earthquake zone and perpetual aftershocks - and also out of the unending rain.
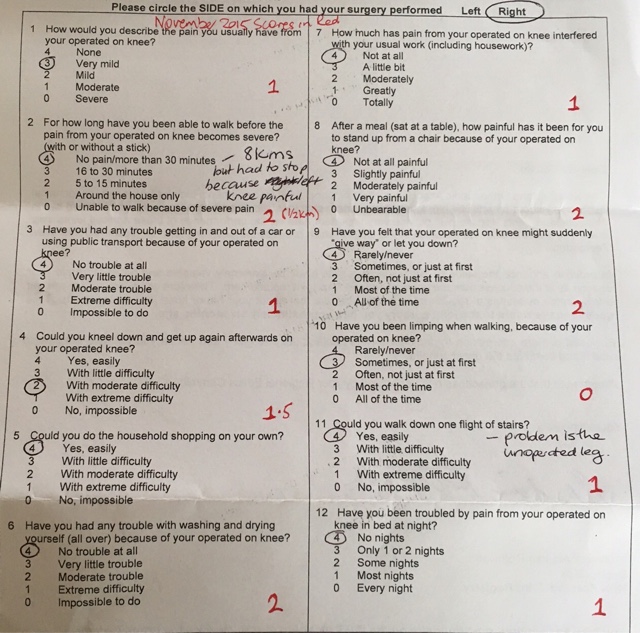
Overall, I would say that this surgery feels quite different from the first knee replacement. To date, the recovery is much speedier, the bruising is resolving faster and wasn't as extensive. I am able to sleep well and I have a greater range of motion in my leg. So - despite the small glitch with the boil - things are looking very promising.